Self-care is a buzzword that’s mentioned a lot these days, but I feel like the meaning can get lost when tossed around so frequently. What does self-care really mean? Care of oneself, sure, that’s easy. We eat, we drink, we sleep – our needs are met, we are cared for. Right?
“Self-care” can be defined as intentional actions that you take in order to care for your own physical, mental, and emotional wellbeing. While eating, drinking, and sleeping would all technically be considered self-care, I’d like to explore the idea a bit further than the basics to stay alive. Our bodies are generally pretty good at making sure our physical needs are met, so what often falls by the wayside is our mental and emotional wellbeing. Here are some approachable and affordable suggestions for incorporating more self-care activities into your daily routine:
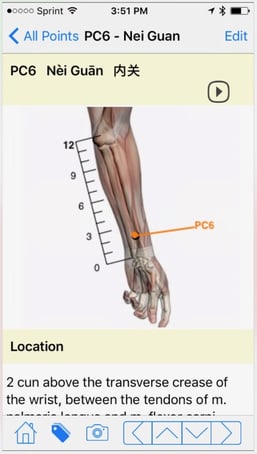
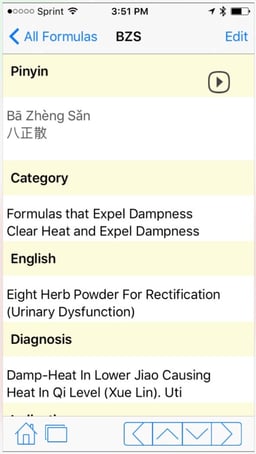
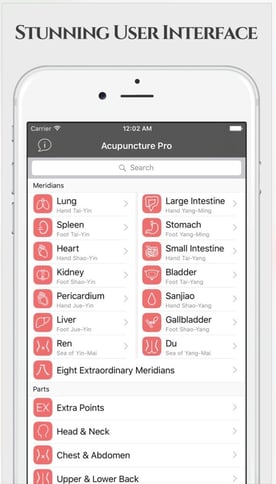
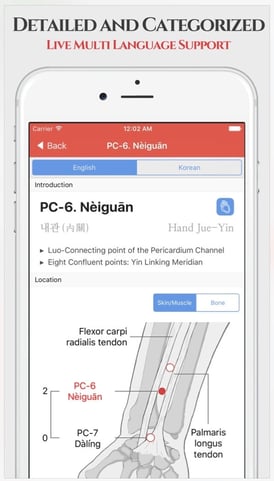
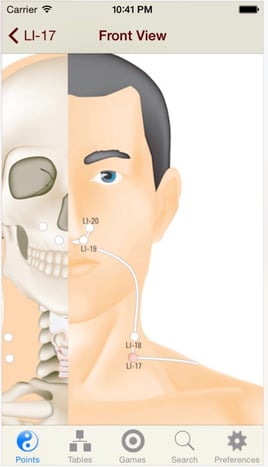
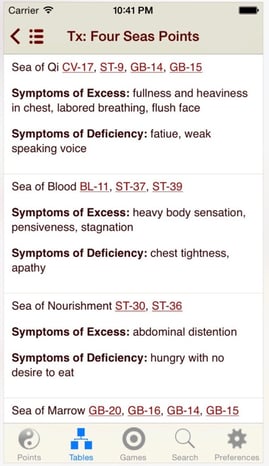
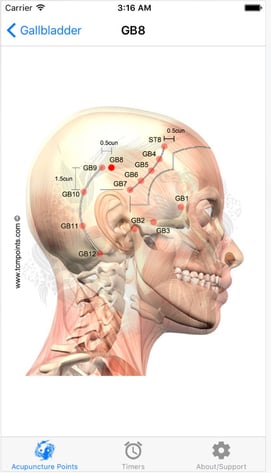
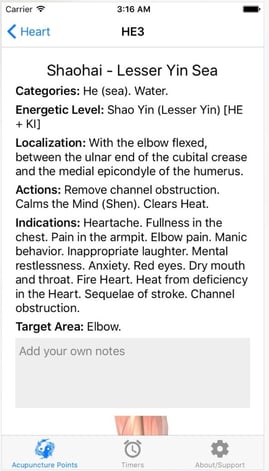
1. Get Acupuncture
Being poked by needles may not be the first item on your “self-care and relaxation” to-do list, but it should be. Hear me out! Symptoms of stress can manifest physically (fatigue, muscle tightness, insomnia, illness, etc.) or emotionally (depression, anxiety, mood swings, poor concentration, etc.) and vary greatly from person to person.
Acupuncture acts on areas of the brain known to reduce sensitivity to pain and stress, also promoting relaxation and deactivating the 'analytical' brain, which handles anxiety and worry (www.acupuncture.org). Research done on a specific acupuncture point (yintang) has shown that, when used during acupuncture or acupressure, this particular point lowered the reported stress levels of volunteers (Fassoulaki). Other research done on the success rates of In Vitro Fertilization, or IVF, found that women undergoing acupuncture combined with IVF had higher successful implantation rates compared with those who did not receive acupuncture (Balk). The World Health Organization lists physical stress symptoms such as fatigue, sleep disturbances, depression, and pain among the problems that acupuncture has proven effective in treating. You can receive acupuncture when these symptoms arise or go in for regular "preventative" visits to stay ahead of any imbalances.
2. Meditate
For many people, meditation might be the most intimidating item on this list. I used to think of meditation as something completely unapproachable, something that only tai chi masters and yoga gurus have the discipline to do. I thought meditation wasn't for me. Not true! I’ve since found that simple, approachable meditation practices such as “Alternate Nostril Breathing” (below) can be effective at reducing stress and bringing my awareness back to the present. Also, apps like Buddhify and Headspace offer a variety of guided meditations for all moods and situations, and you can always check out a class at AOMA! Every Sunday evening from 5-6pm there is a free meditation class at the AOMA South campus - no registration or materials are required.
Alternate Nostril Breathing:
• In this exercise, the breath should be relaxed, deep and full.
• Use the thumb of the right hand to close the right nostril, and the index finger or ring finger of the right hand to close the left nostril.
• Close the right nostril and inhale through the left nostril.
• Then close the left nostril and exhale through the right nostril.
• Then inhale through the right nostril.
• Close the right nostril and exhale through the left nostril.
• Continue repeating, alternating nostrils after each inhalation.
• Inhale left, exhale right: helps to make you calm and integrates unwanted negative emotions and stress, excellent by itself before bed.
• Inhale right, exhale left: Gives clarity and positive mood, helps us to focus on what is important. (www.3ho.org)
3. Exercise
Aerobic exercise causes your brain to produce more endorphins, which are the body's natural painkillers and "feel-good" neurotransmitters. Exercise also maintains both physical and mental fitness, reduces fatigue, improves alertness and concentration, and enhances cognitive function. It doesn't have to be high-intensity or long-duration; even just 5 minutes of aerobic exercise can stimulate anti-stress effects (www.adaa.org). My personal recommendations include yoga, qigong, tai chi, walking, running, or swimming, but any activity that inspires you to get up and get moving is perfect! Studies have shown that both brisk walking and tai chi can reduce levels of the stress hormone cortisol and improve mood (Putai).
4. Hydrate
This is the easiest item on the whole list yet the one that I struggle with the most! All our organs need water to function, and studies have shown that being just a half-liter dehydrated can increase your body's cortisol levels (Shireffs). Stress also causes your body to release more water by elevating your heart rate and increasing both ventilation and perspiration (Maresh). Drinking a glass of water won'tmake your problems disappear, but dehydration will make you feel worse! Keeping your body fully hydrated will enable you to perform better under pressure and may help you feel less stressed. I use an app called Plant Nanny that reminds me to hydrate throughout the day and helps me track my daily water intake in a cute, fun way.
5. Think Happy Thoughts
An important aspect of self-care is thinking about and focusing on things that inspire you to feel more positive and hopeful. Research has shown that negative thinking can both produce and sustain depression, which can then affect memory and cognitive brain function (Teasdale). There’s a quick and easy “positive words” exercise that I like to do in the mornings, sometimes while the coffee is brewing or even before I even get out of bed. I stand or lay quietly for a minute or two and brainstorm a list of random positive words – no order, no logic, no pressure – just a free-flow of any positive words that come to mind. It can be challenging some days but it’s always fun, and most of the time I’m smiling before I even realize it. Typically I don’t write anything down, but this morning I did so that I could share my list with you:
|
Laugh
|
Smile
|
Abundance
|
Love
|
Share
|
|
Joy
|
Mercy
|
Compassion
|
Inspired
|
Blessing
|
|
Happy
|
Fulfilled
|
Embrace
|
Brave
|
Enjoy
|
|
Thankful
|
Goal
|
Accomplish
|
Success
|
Friend
|
|
Brilliant
|
Positive
|
Giving
|
Awesome
|
Connected
|
|
Sunshine
|
Ready
|
Cherish
|
Healthy
|
Fun
|
Making this list took me just 3 minutes; I smiled while I was writing it and I’m smiling again as I re-type it now. Try it for yourself! It’s amazing how powerful a few words of affirmation can be when they brighten your day and remind you of the positivity that already exists inside your own head.
6. Bonus Tip: Ask for Help
If you try all the items on this list and don't feel any positive improvements in your sense of wellbeing, it may be time to look outside yourself for help. Reaching out to a trusted friend or another member of your support system might help, or you may need to seek the advice of a qualified medical professional like a therapist or counselor. Your body might also be trying to tell you something, and a visit to your primary care physician could reveal an underlying medical cause for your symptoms. Please feel free to contact the AOMA Clinics for recommendations on local acupuncture-friendly physicians and specialists.

Resources:
Balk, Judith, et al. “The relationship between stress, acupuncture, and IVF patients: a pilot study.” Complementary Therapies in Clinical Practice. Volume 16, Issue 3, August 2010, Pages 154–157
Fassoulaki, Argyro, et al. “Pressure Applied on the Extra 1 Acupuncture Point Reduces Bispectral Index Values and Stress in Volunteers.” Anesthesia & Analgesia: March 2003 - Volume 96 - Issue 3 - pp 885-890
Maresh, C.M. et al. "Effect of Hydration State on Testosterone and Cortisol Responses to Training-Intensity Exercise in Collegiate Runners." Int J Sports Med 2006; 27(10): 765-770
Pomeranz, Bruce. “Scientific Research into Acupuncture for the Relief of Pain.” The Journal of Alternative and Complementary Medicine. August 2007, 2(1): 53-60.
Putai, Jin. "Efficacy of Tai Chi, brisk walking, meditation, and reading in reducing mental and emotional stress." Journal of Psychosomatic Research, Volume 36, Issue 4, May 1992, Pages 361–370
Shirreffs, S M. "Markers of Hydration Status" Journal of Sports Medicine and Physical Fitness 40.1 (Mar 2000): 80-4.
Teasdale, John D. “Negative Thinking in Depression: Cause, effect, or reciprocal relationship?” Advances in Behaviour Research and Therapy. Volume 5, Issue 1, 1983, Pages 3–25
www.adaa.org/understanding-anxiety
https://www.3ho.org/files/pdfs/alternate-nostril-breathing.pdf
http://www.acupuncture.org.uk/a-to-z-of-conditions/a-to-z-of-conditions/stress.html
http://johnsoncook.com/positive-words-exercise-nobody-is-watching/#.V30_SfkrKUk